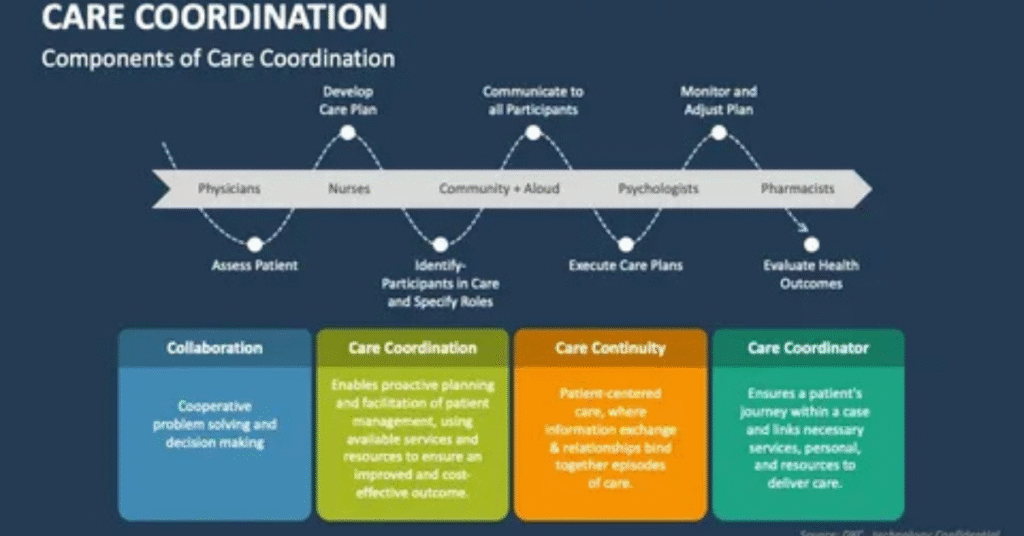
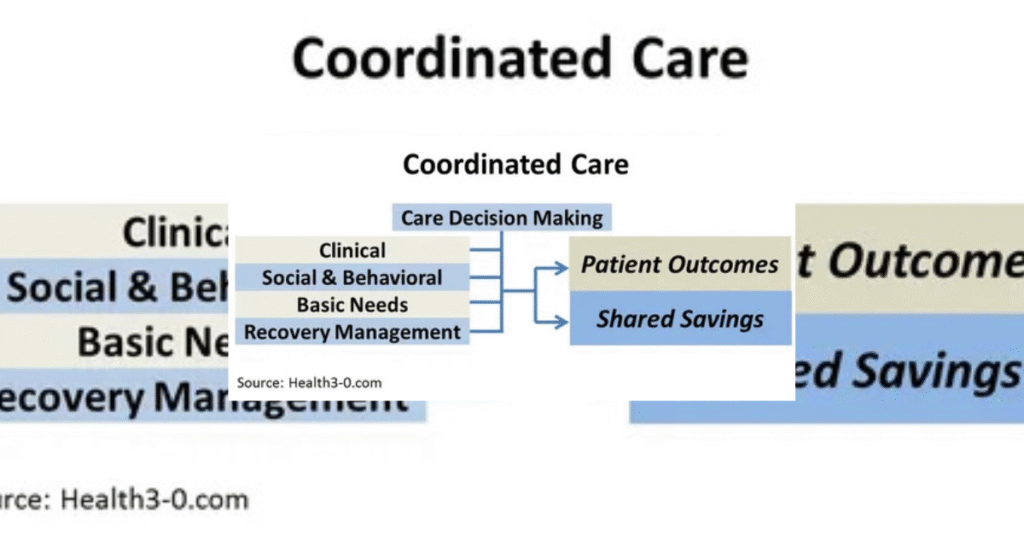
The role of a care coordination plan in healthcare cannot be overlooked in the modern world. Patients tend to see various doctors, hospitals, and specialists. Without any planning, this can lead to confusion, money spent unnecessarily, and dangerous gaps in treatment.
A care coordination plan ensures that all the people involved in the care of a patient coordinate with each other. It links doctors, nurses, and families so that the patient receives appropriate treatment at the appropriate time. When care is uncoordinated, patients are likely to duplicate tests, forget medications, or get admitted to the hospital again. That is why coordinated care is the foundation of safe and contemporary healthcare.
What Is a Care Coordination Plan?
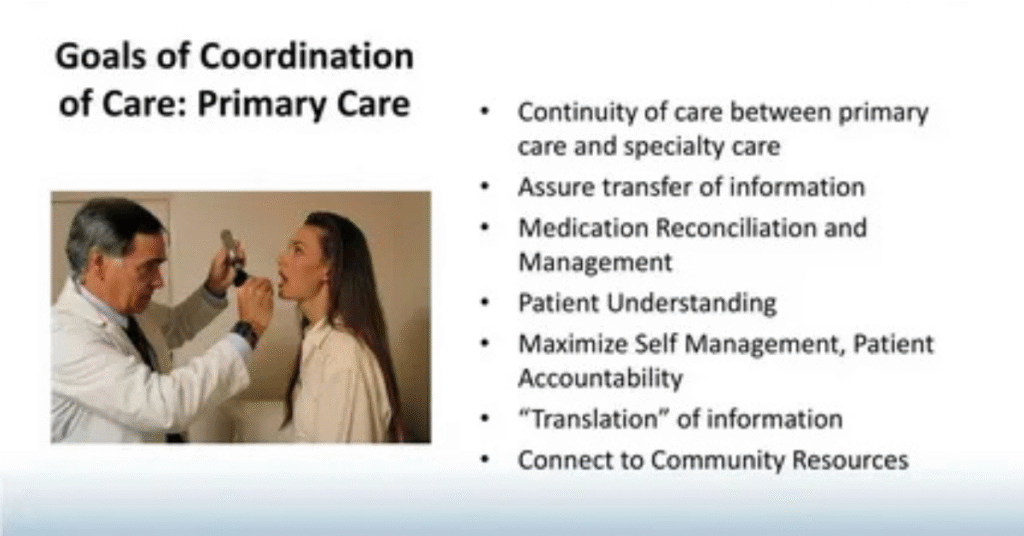
A care coordination plan is a structured method that helps manage a patient’s care across many healthcare providers. It makes sure that information flows smoothly from the family doctor to the specialist, from the hospital to the home nurse, and back again.
This plan usually includes details about the patient’s health goals, medicines, schedules for follow-up visits, and emergency instructions. It is more than just paperwork. It is a living guide that evolves as the patient’s condition changes. Care coordination is especially vital for people with chronic illnesses, disabilities, or those recovering from major surgery.
Why Care Coordination Matters in Healthcare

Healthcare systems are often fragmented. A patient may see one doctor for the heart, another for diabetes, and yet another for mental health. Without communication, treatments overlap or clash. A care coordination plan prevents this by creating a single roadmap for all providers.
Good coordination also improves safety. For example, when doctors share records, the risk of harmful drug interactions drops. Patients feel more supported when their providers work together rather than separately. In this way, a simple plan can protect lives while making care smoother and less stressful.
SEE MORE: https://doctorambulance.com/how-much-will-an-ambulance-ride-cost-a-complete-guide/
Benefits for Patients

Patients are the biggest winners when care is well coordinated. They enjoy shorter hospital stays, fewer repeated tests, and fewer emergency visits. For example, an elderly patient with heart disease and arthritis can avoid unnecessary stress when one doctor updates another about their medications.
Patients also gain confidence when they clearly understand their treatment plan. A care coordination plan explains in plain words what medicine to take, when to take it, and what warning signs to look out for. This support helps patients stay healthier and avoid preventable complications.
Benefits for Healthcare Providers
Doctors, nurses, and specialists also benefit from care coordination. Clear communication reduces mistakes and misunderstandings. Providers save time because they don’t need to repeat tests or search for missing records.
A good plan also lowers stress for healthcare staff. Instead of feeling isolated, they become part of a team working toward the same goal. This teamwork improves job satisfaction and reduces burnout, which is a serious problem in modern healthcare. Providers who work in a coordinated system often report that they can focus more on patient care rather than paperwork.
System-Level Impact on Healthcare

At a broader level, care coordination transforms healthcare systems. It reduces waste, saves money, and improves efficiency. Hospitals spend less on readmissions because patients are less likely to return for the same problem. Insurance companies and governments also save when unnecessary treatments are avoided.
Coordinated care supports value-based care models, where payment is linked to outcomes rather than the number of services delivered. This shift pushes healthcare systems to focus on prevention and long-term health instead of only treating emergencies. Over time, this leads to healthier communities and stronger public health.
Cost Impact of Care Coordination
| Aspect | Without Care Coordination | With Care Coordination |
| Hospital readmissions | High | Lower |
| Duplicate tests | Frequent | Reduced |
| Medication errors | Common | Rare |
| Patient satisfaction | Low | High |
Common Challenges in Implementing Care Coordination Plans
Even though the benefits are clear, building a care coordination plan is not always easy. Communication gaps remain one of the biggest barriers. Doctors in different facilities may not share the same systems or even speak directly to one another. This creates dangerous blind spots.
Time and staffing are another issue. Busy healthcare teams often struggle to sit down and plan carefully for each patient. Patients themselves may add challenges if they do not follow instructions or have limited understanding of their condition. Health literacy plays a huge role in whether coordination succeeds.
The Role of Technology in Care Coordination
Technology is a powerful tool for solving these challenges. Electronic Health Records (EHRs) allow providers to access updated patient information instantly. Telehealth makes it possible to check on patients without requiring them to travel.
Patient portals and mobile apps remind people about their medicines and appointments. Artificial intelligence is now being used to predict which patients are at higher risk of readmission. By alerting doctors early, these systems prevent small problems from turning into major ones.
Technology Supporting Care Coordination
| Technology Tool | Function in Care Coordination |
| Electronic Health Records | Central storage of patient data |
| Telehealth | Remote monitoring and care |
| Mobile Apps | Medication and appointment reminders |
| AI Predictive Analytics | Identifying high-risk patients |
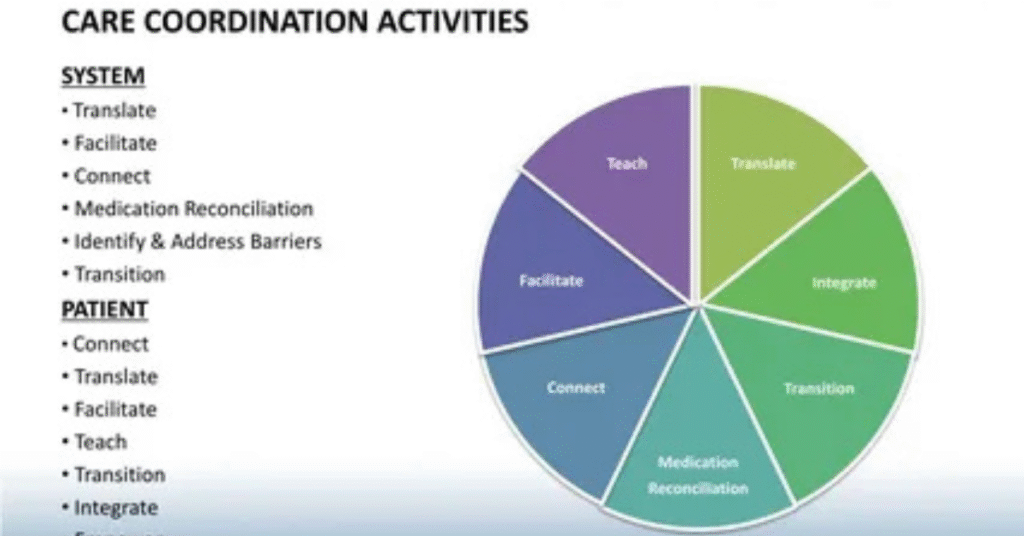
Practical Strategies to Improve Care Coordination
Improving coordination requires both planning and teamwork. Hospitals can form multidisciplinary teams where doctors, nurses, pharmacists, and social workers work side by side. This allows for a complete view of the patient’s needs.
Standardized discharge planning also makes a big difference. Patients should leave the hospital with clear instructions, follow-up dates, and contact information. Training providers in communication skills and engaging patients in decision-making helps create trust and better outcomes.
Case Example: Successful Care Coordination in Action
A strong example of effective coordination comes from a program for heart failure patients. Hospitals that created personalized care plans saw dramatic results. Patients were given digital devices to track weight and blood pressure at home. Nurses monitored the data and contacted patients if there were early warning signs.
This program reduced hospital readmissions by nearly 30 percent in one year. Patients felt safer, and nurses reported less stress. This case shows how a simple but structured care coordination plan can save lives and lower costs.
Future of Care Coordination

The future will bring even more reliance on digital tools. Artificial intelligence will likely guide treatment choices and prevent errors. Preventive care and community health programs will become central, reducing the need for emergency services.
Government policies and insurance models are also shifting to reward care that is coordinated, not fragmented. Over the next decade, the importance of a care coordination plan in healthcare will grow even stronger. Patients will expect it as a standard, not a luxury.
Future Trends in Care Coordination
| Future Trend | Expected Impact |
| AI-driven planning | Personalized care |
| Preventive care focus | Lower hospital use |
| Policy support | Wider adoption |
| Community-based programs | Stronger public health |
Policy Support for Care Coordination
Government policies play a major role in making care coordination stronger. In many countries, health authorities now push hospitals and clinics to share patient data and follow common standards. Programs like Medicare in the United States reward providers when they prevent readmissions through better planning.
This shift shows that care coordination is not only good practice but also a requirement. When policies and funding support these systems, hospitals and clinics are more motivated to build structured plans that keep patients safe and healthy.
Patient Involvement in Care Coordination
Patients are not just passive receivers of care. Their involvement is key to the success of any care coordination plan. When patients understand their medicines, appointments, and lifestyle changes, they are more likely to follow through and stay healthy.
Engaging patients also builds trust. For example, allowing them to access their medical records online or involving them in decision-making makes them feel part of the team. A plan that includes the patient’s voice always leads to better results.
YOU WILL LIKE: https://doctorambulance.com/do-ambulance-lights-turn-off-when-someone-dies/
Training and Education for Providers

Even the best technology cannot replace well-trained providers. Doctors, nurses, and support staff need constant training on how to communicate and work as a team. Many hospitals now run workshops that focus on patient-centered communication and cultural sensitivity.
Education also extends to using digital tools. When providers know how to use electronic records and telehealth properly, the coordination plan becomes smoother and more reliable. Skilled staff are the backbone of successful coordinated care.
Measuring Success of Care Coordination Plans
A care coordination plan must be measured to know if it is working. Hospitals often track readmission rates, patient satisfaction surveys, and medication error reports. These numbers reveal whether the plan is making a real difference.
Regular evaluation helps in spotting weak areas. For example, if patients still miss follow-up visits, the hospital can improve reminders. By measuring outcomes, providers make sure that coordination is not just an idea on paper but a proven system that delivers results.
Conclusion
The importance of a care coordination plan in healthcare is clear. It connects patients, providers, and systems into one smooth network. It saves time, prevents mistakes, and helps patients feel supported. With technology and teamwork, care coordination is shaping the future of healthcare. In simple words, it is the bridge between confusion and clarity, and it ensures that every patient receives safe, complete, and compassionate care.
FAQ”s
What is the purpose of a care coordination plan?
Its purpose is to connect healthcare providers and guide patients through treatment with fewer errors and better outcomes.
Who benefits the most from care coordination?
Patients with chronic illnesses, the elderly, and those with complex medical needs benefit the most.
How does care coordination reduce healthcare costs?
It prevents unnecessary tests, lowers hospital readmissions, and avoids medical errors that cost money.
What role does technology play in care coordination?
Technology like EHRs, telehealth, and mobile apps makes communication and patient monitoring easier and faster.
Is care coordination only for hospitals?
No, it is useful across all settings including clinics, home care, nursing homes, and community health programs.
Pingback: Are Ambulance Rides Covered by Insurance? - Doctor Ambulance Are Ambulance Rides Covered by Insurance?